October 1989. Reston, Virginia, the US. Population: 49,000. A man is taking out the trash and sees three white vans speed past. For a casual bystander, there’s no way of knowing that the unmarked vans are transporting a dozen soldiers to a mission that is highly unusual – and highly unsettling.
The vans drop the army biohazard team at a weathered building, where they reluctantly change clothes before entering, stripping to the skin and suiting up. Wearing bright orange hazmat suits pressurised with a six-hour supply of filtered air, they enter the building. The fierce cries of the enemy can be heard echoing through the halls: dozens of sick, starving macaque monkeys in cages, eyes bloodshot, teeth bared. The military biohazard team is there to put the primates out of their misery – or, as the lead scientist put it, “depopulate the facility”.
The lights are off in the quarantine facility and the climate control systems are malfunctioning. The team are soon dripping with sweat inside their uninsulated suits, and everyone knows the risk: a single tear in your suit could be a death sentence.
The disease raging inside these test monkeys, imported from the Philippines, is as diabolical as their frenzied, reddened eyes. “Zaire Ebola”, one of the deadliest viruses in the world, is supposedly only found in Africa, but an outbreak has suddenly reared its head here, in the US, just a 30-minute drive from the nation’s capital.
We are waking up to a world where pandemics are possible
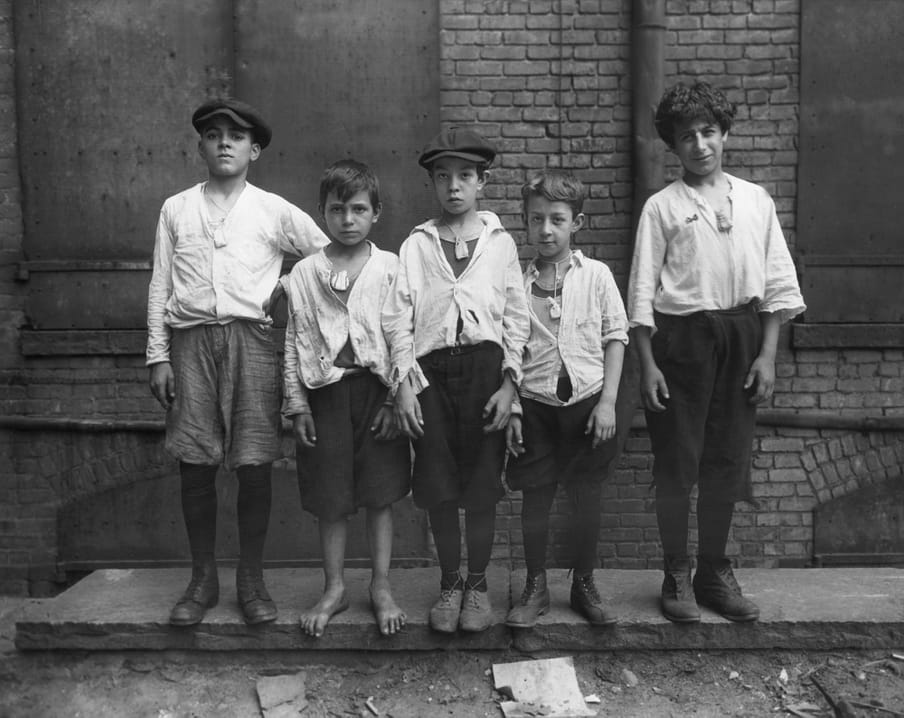
These are images from a 2019 miniseries called The Hot Zone, which had me glued closer to my screen than anything else that caught my attention in these times of Netflix gluttony. The series was based on the 1994 book of the same title by New Yorker journalist Richard Preston. The book describes the outbreak of what is now known as “Reston ebolavirus”, a strain of the virus that (spoiler alert!) was initially thought to be Zaire Ebola, but later proved to be a different variant which was only lethal to primates. Why? No one knows.
The underlying message of the miniseries – that the outbreak could just as easily have ended much less quickly – hits hard in the midst of what’s happening now, even though I have caught myself enjoying reading about historical pandemics and disease outbreaks over the past few weeks. Whether it’s consolation or something more perverse, I don’t know.
What I do know is that people are becoming aware that pandemics are possible: in our own countries, on our own streets. In my case, that awareness has been accompanied by a renewed sense of awe – something that smarter minds than mine have been emphasising for ages. Once this miserable situation is over, I said to my girlfriend, we’re going to Micropia, a museum in my home city dedicated to microbes. To bow humbly to the mighty microbes and pathogens.
But viruses like Sars-CoV-2 are more than microscopic particles.
I realised that last week, while devouring The Pandemic Century : One Hundred Years of Panic, Hysteria and Hubris (2019) by Mark Honigsbaum, a British journalist and medical historian. The book shows that many epidemics feature an overwhelming history.
Honigsbaum takes his readers on a tour of the most striking pandemics and epidemics since the Spanish flu in 1918. Although these cruel diseases were completely different in scope and influence, the outbreaks do have some things in common. They force us to face the limitations of medical paradigms, they’re always related to how humans influence their surroundings, and they consistently foster both hysteria and hubris.
How the war assisted the Spanish flu
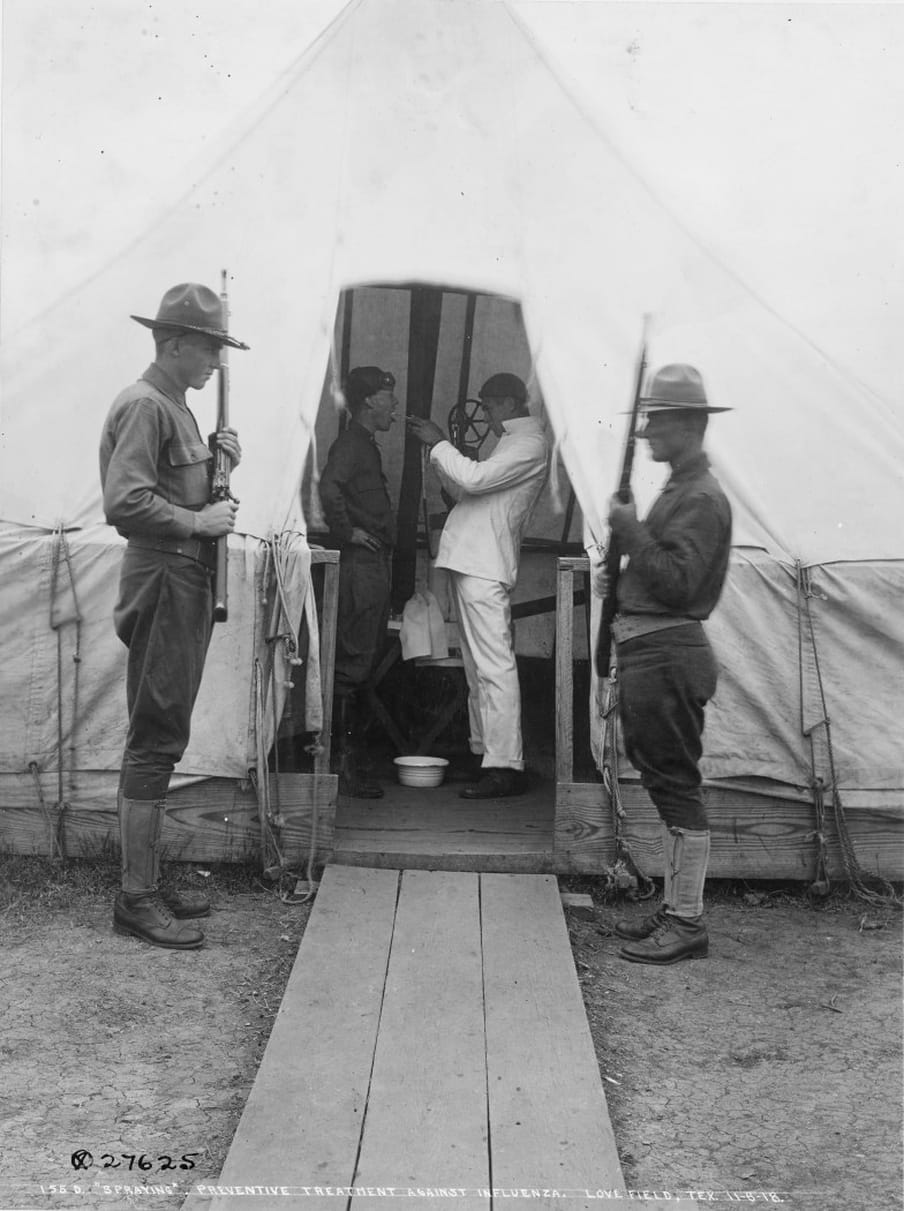
The journey begins in 1918. In a military training camp in Massachusetts, thousands of young recruits were preparing to head out to fight overseas. It was cold, filthy and overcrowded, and – just like in war-ravaged Europe – a respiratory infection was sweeping through the throngs of young men. The symptoms included high fever, extreme shortness of breath and lips tinged ominously blue. There was no treatment.
The unknown disease was soon known as the “Spanish flu” and would ultimately claim the lives of 675,000 US Americans. Estimates put the global death toll somewhere between 50 and 100 million, making it the deadliest epidemic in human history.
No one knows exactly where that wartime winter’s outbreak originated, but the virus was probably spread by troops returning from the frontline of the first world war. The trenches of northern France made for a gigantic ecological experiment, with throngs of people from all around the world – with all sorts of immune systems – converging on that one region.
Bacteria were initially blamed for the disease. Honigsbaum describes how stubborn scientists, convinced of the “bacterial paradigm”, made every effort within their power to see that assumption confirmed. In reality, influenza A is a viral infection. This was only definitively proven in 1933 when an infected ferret sneezed on a laboratory technician, who then fell ill. The virus – H1N1 – was not visible through a microscope until the 1940s. And it wasn’t until 2005 that scientists mapped its entire genome and discovered that its origins could probably be traced back to bird populations.
The enormity of so many deaths from one disease is difficult to imagine now. But perhaps the most breathtaking aspect of the Spanish flu was that it killed so many young people. Until then, the seasonal flu had mainly affected young infants and the elderly, but people aged 20 to 40 were a major risk group in that pandemic. Why? To this day, there’s no conclusive proof.
Honigsbaum’s story primarily shows how closely the pandemic was linked to war, which is often the case: “Ever since Pericles ordered Athenians to sit out the Spartan siege of their harbor city in 430 BC [during which there was an outbreak of plague], wars have been seen as progenitors of deadly outbreaks of infectious disease.”

Deadly ornamental birds fly all over the world
That darkest of pathogens, the Black Death, has hit communities hard across the ages – and not just in antiquity and the middle ages.
In 1924, not long after the Spanish flu had come and gone, the plague turned up in the overcrowded Mexican quarter of Los Angeles. Local residents developed a high fever, a nasty cough and an aggressive pneumonia, and a few succumbed quickly to the disease. During the open-casket funeral of one of those early victims, many of those present kissed the deceased woman farewell according to Catholic custom, allowing the disease to spread like wildfire among the grieving relatives.
The mythical bacterium responsible for the plague, “Yersinia pestis”, has historically claimed as many as 200 million victims. Y. pestis generally lies dormant, passed around among wild rodents, such as rats, without causing any further harm. However, if rats catch the disease and then come into contact with humans, there is a risk of transmission via fleas.
The health of rodent populations is actively monitored these days. Plague periodically crops up every now and then, but can now be treated effectively with antibiotics. The people in that poverty-stricken, densely populated Mexican quarter did not have access to such solutions. The outbreak was contained only by strict quarantine measures that would be considered downright racist by today’s standards.
The close ties between infectious diseases and our relationship with animals became apparent again a few years later, when the world was hit by a new pandemic. But the culprit this time was far lovelier in appearance than the lowly feral rats.
In the 1930s, exotic birds were in great demand all around the globe. For widows and bored housewives, parakeets and canaries were “the FM radios of their day”, Honigsbaum writes. Hundreds of thousands of birds were shipped from distant tropical climes to wealthy countries in the west. No one suspected that those new-found feathered friends carried a bacterium that could cause pneumonia. But in 1929, cases of “parrot fever”, or psittacosis, were reported all over the place, from Argentina to Switzerland and from Holland to Honolulu.
An important insight that this pandemic would bring, Honigsbaum writes, is that wild birds in nature pose virtually no risk to humans. Parasites circulating in wild populations actually benefit the overall equilibrium. Problems only arise when people disturb this biological balance by packing birds in cramped crates for shipping. And that doesn’t apply to just birds.
Parrot fever would serve as a lesson for the increasingly globalised future. Overpopulation, global aviation, international trade and factory farming: it’s becoming more common for pathogens to make the jump from animals to humans, a factor that we are painfully reminded of today in our well-informed home quarantines.
As early as the 1930s, scientists already feared that rapid economic and industrial developments would disturb the delicate balance between man and microbe. That fear would become a reality, for example in the 1970s, when the “Philly Killer” struck in Philadelphia.

The silent killer in the hot tub
Throughout the 18th and 19th centuries, pneumonia was widely feared above almost all other diseases. But as antibiotics became widely available, that changed in the 1950s and 1960s. People started to believe that infectious diseases had been vanquished for good. Prompted by aggressive advertising for cleaning products and shiny surfaces, US Americans envisioned themselves as embarking on a “germ-free era”.
But such proclamations proved to be premature in the summer of 1976, when thousands of war veterans attended a four-day convention in a luxury hotel in downtown Philadelphia. They congregated in the hotel’s huge ballrooms and spacious terraces to dine, drink and socialise.
A week later, six veterans in the greater Philadelphia area were seriously ill and one had died. Across the US, people who had attended the convention showed up in hospital with – you guessed it – pneumonia.
It wasn’t influenza, as it turned out, nor the swine flu, as was initially feared by people who were already concerned about a potential outbreak of that virus. Everyone breathed a sigh of relief several weeks later when it became apparent that it wasn’t contagious; no secondary cases were reported. But the ailment that had befallen the veterans was still a mystery, and would remain so for some time.
Two years later, it would become apparent that the disease contracted by the veterans was, in fact, directly related to the chic hotel.
Legionella pneumophila, as the bacterium that made them sick would be named, is found in water, particularly water that’s home to other organisms which it can parasitically live off. Under natural conditions, water does not generally reach temperatures that allow bacteria to multiply rapidly, but human-made environments are a whole different story. Hotels, hospitals and other large urban buildings are equipped with systems that keep water at comfortable, usable temperatures, providing an ideal environment for legionella to breed.
It is a classic example, Honigsbaum emphasises, of how new technologies and changes to the built environment – in this case, actually designed to promote hygiene – are constantly accompanied by new health risks.
Anyone who still cherished the illusion that infectious diseases had been banished to the annals of history, even after the panic prompted by the discovery of legionnaires’ disease, would shortly see their illusory bubble popped for good. An unprecedented and merciless assassin was already nestling unnoticed in the bodies of healthy young people all over the world.

HIV
When should we pinpoint the origins of the Aids virus in human history? We could start with chimpanzees in inland Cameroon, for instance, or with Gaëtan Dugas, the Canadian flight attendant who was initially thought to have been “Patient Zero”. Honigsbaum starts in December 1980, in a Los Angeles hospital, when 33-year-old artist Michael ended up in the emergency room. He was emaciated and had thrush, a yeast infection of the mouth and throat, usually indicative of immune deficiency.
Michael was admitted to hospital in March of the following year, but no treatment they tried had any effect; he died of pneumonia in May 1981.
Doctors in LA and New York saw many more men that winter who, like Michael, had thrush and often exhibited additional symptoms such as fever, diarrhoea, swollen lymph nodes and dark skin lesions, indicating a rare form of skin cancer known as Kaposi’s sarcoma. Like Michael, most of the patients were gay men.
Within a few months, these worrying symptoms would grip the whole world in fear. In 1982, 4,000 deaths were reported in the US alone from what had by then been labelled “acquired immunodeficiency syndrome” (Aids), the disease caused by the human immunodeficiency virus (HIV). By the end of the 20th century, 14 million people had been infected with HIV worldwide; by now, that figure has risen to 40 million, most of them on the African continent.
At first, Honigsbaum explains, the public responded to the new disease with resounding indifference – partly out of ignorance and partly out of the persistent prejudice that Aids only affected gay men. In the first few years of the epidemic, Ronald Reagan, the president, refused to use “the A-word” and denied funding for Aids researchers.
It was not until 1985, by the time that Aids had been diagnosed in 10,000 Americans, including children and haemophiliacs, that panic truly took hold. By that point, it had become clear that HIV was transmissible through blood, that the virus could spread via shared needles, and that the national blood supply had been contaminated. The euphemistic term “bodily fluids” used in government information gave people the impression that they could catch the virus from saliva or sneezing, or even from touching all sorts of surfaces. And word got out that heterosexual people could also infect each other during sex.
Honigsbaum’s account shows how incredibly complex the history of Aids is. It highlights how social, cultural, geopolitical, geographical and biological factors interact over vast periods of time.
For example, besides all kinds of complicated analyses about the zoonosis of the virus, the Aids pandemic was partly the result of colonial-era infrastructure that connected various parts of central Africa. As a result, men flooded into the countryside in search of work, gender relations were destabilised, and a culture of prostitution emerged in large cities such as Léopoldville (now Kinshasa).
The loosening of sexual morals was also hugely significant in the spread of the virus in the US and Europe – especially in cities like New York and San Francisco, where bathhouses and saunas became cruising hotspots for the hedonistic gay scene. But, warns Honigsbaum, there are quite a few caveats to that well-known and socially stigmatising story.
Dismissing Aids as “a gay disease” was a ridiculous oversimplification, as it turned out, but that discriminatory assumption did inform initial reactions and shaped the course of events.
Hysteria and hubris
Just like the Aids epidemic, which initially met with lukewarm indifference from the government, only to later lead to mass hysteria, nearly all of the pandemics that Honigsbaum describes were surrounded by either denial or panic. Apparently, it’s almost impossible to accurately assess the real impact of an outbreak from the outset, which is precisely what makes epidemics so susceptible to contradictory reactions. We can observe this phenomenon in real time right now in the fluctuating alarmism expressed by world leaders.
Obviously, the media also plays a role here. During the 1924 outbreak of plague in Los Angeles, almost no one living in LA had any idea of the drama unfolding in the Mexican quarter in their own backyard. Local authorities downplayed the situation to the outside world to avoid panic. In New York, on the other hand, the outbreak on the west coast was front page news, not least because prominent headlines shouting about "plague!” were brilliant for newspaper sales.
A few years later, parrot fever did cause considerable panic. But it wasn’t until 1976, when the failing mayor of Philadelphia seized upon legionnaires’ disease as a pretext for sowing fear of a terrorist attack, that the full potential for politicising a public health crisis became apparent. The mayor’s press secretary was all set to feed the press a conspiracy theory about the CIA, alleging that the US intelligence agency had secretly been developing biological weapons (just like Trump supporters today claiming that the coronavirus is a Chinese bioweapon).
At the same time, journalists were wondering if the mystery illness killing the war veterans from the American Legion convention had been the plague, while other politicians grabbed their chance to sow paranoia about the pacifist movement by suggesting that the outbreak could be the work of a frustrated veteran gone rogue with a home chemistry set.
The surge in pandemics in the 21st century also reveals how many geopolitical interests now play a role in this complex web of factors. Transnational bodies such as the World Health Organization (WHO) are indispensable in the response to infectious diseases. Scientists and labs from all over the world are now involved in research on precise identification of any potentially novel virus that emerges.
Despite all this, governments still manage to conceal outbreaks and disseminate disinformation. Until recently, Russia was still denying any spread of Covid-19 within its borders. Back in 2003, it was a similar story: it took the Chinese government months (and a whistleblower who forced the issue) to reveal how many Chinese people were actually suffering from a new, typically 21st century virus: Sars.

The jetset disease
The 21st century had barely started when the WHO picked up indications in February 2003 that there was an unusual outbreak of respiratory infections in Guangzhou, a Chinese city with a population numbering in the millions. The WHO received reports that face masks were being hoarded in Guangzhou, and there was a major run on antibiotics and white vinegar (used in traditional Chinese medicine).
At first, scientists thought this must be the bird flu that they had been anxiously anticipating. However, initial testing told a very different story. Hundreds of labs all over the world were mobilised and entire hospitals filled with infected patients before it was identified a few months later. By that point, the disease had made it all the way to the other side of the world: Canada.
The culprit turned out to be a coronavirus that had never been seen in humans before. The virus was highly contagious, and scientists and healthcare professionals were reluctant to handle contaminated blood samples and work with infected patients.
Although the world’s attention was initially focused on the war in the Middle East, Sars soon dominated the news cycle. Toronto, which had an outbreak in a hospital, was gripped by widespread panic, but the epidemic was an absolute disaster for Hong Kong. TV broadcasts showed terrifying images of men wearing hazmat suits cordoning off a large residential complex and placing it under armed guard.
This wasn’t an animal flu after all, it was “Severe Acute Respiratory Syndrome”, a virus that sounded much more urban than “bird flu” – and therefore more threatening.
Sars came to be known as the first “jetset disease” of the new millennium because of how fast it hitchhiked throughout Asia and then hopped to Canada via air traffic. Spreading around the globe even faster than the virus in these hyperconnected times, the news had the whole world as a captive audience.
In other words, the new global world order was assisting the spread of the virus. But how had it emerged from a family of coronaviruses that was normally only found in animals?
In order to find out, researchers had to take their swabs to the market – more specifically, the “wet markets” which, according to Chinese custom, sold a wide array of exotic animals, from raccoon dogs and Chinese hares to ferret-badgers and civet cats. Masked palm civets turned out to be the carriers. What’s more, the merchants that sold them tested positive for antibodies, which indicated that the virus had been circulating between humans and animals for some time.
But that’s not where the search ended. In 2005, it turned out that the civet cats were only stepping stones; the true reservoir of the virus turned out to be bats – horseshoe bats, to be precise.
“I think people should stop hunting and eating bats,” one of the researchers concluded. The same rule was applied to civet cats, a popular delicacy in the region. Although China temporarily banned the animals after the Sars outbreak, they eventually reappeared on the menus of exclusive restaurants.
A hunger for exotic sources of protein, assisted by more frequently and even faster air transport, had given Sars the chance to infect around 8,500 people worldwide and kill 900.
And here’s where the story starts to blend into our present predicament.
Bats are also now being mentioned as possible hosts for the current coronavirus, known as Sars-CoV-2, which distinguishes itself from Sars by its coronal halo of “spikes” that help it latch onto human cells even better. And bats are the start of Honigsbaum’s story about the most recent epidemic before Covid-19.
The Ebola epidemic
In December 2013, a small group of children gathered around a hollow tree in Meliandou, a tiny village in south-eastern Guinea. They probed the opening with sticks to drive out the long-tailed bats nesting inside the tree. The flesh of these plump creatures was an important source of protein for the villagers.
Not long after, one of the children (two-year-old Emile) developed a high fever, accompanied by vomiting and diarrhoea. A few days later, he was dead. Emile’s mother and sister followed a week later.
The village was situated close to the road to a trading post; within a few weeks, the nasty disease had spread to the surrounding areas and crossed the border into Liberia. When a doctor from Doctors Without Borders heard from colleagues what the symptoms were, he knew immediately what they were dealing with. He had stared this monster down before: Ebola.
There had been an outbreak of the filovirus some 10 years earlier in the Democratic Republic of Congo (formerly known as Zaire), where it had a mortality rate of 90%. Ebola is one of the most aggressive diseases known to man, as the doctor was well aware, and one of the most frightening. There is no vaccine.
Ebola is less easily transmissible than Sars or HIV, but highly contagious all the same. It poses a particular risk to care workers who may come into contact with blood and vomit from patients who are deathly ill. Patients and care providers alike must be placed into maximum isolation as quickly as possible. But local conditions were suboptimal for such measures, and it would soon become apparent how much people can help a virus along.
A few months after the outbreak, the WHO announced the news. But officials seemed largely unconcerned about an outbreak in the remote forests of Guinea. Even when warned that the virus was spreading rapidly, perhaps even across national borders, high-ranking officials in the WHO did not raise the alert level.
And although there was a lack of effective materials, including tests, local authorities in Guinea instructed doctors only to report officially tested cases.
Another factor that increased the risk in west Africa was traditional burial rites aimed at uniting the dead with their ancestors in the afterlife. These rites involved washing and dressing the corpses and blessing them in a hands-on ritual.
To make matters worse, the medical teams who came to help in their brightly coloured hazmat suits were distrusted and even attacked by the people, who were fiercely dismissive of government authorities after centuries of colonial oppression, exploitation and corruption. As the virus spread, so did the rumour that these suited bioresponse teams were actually infecting people with the disease.
All these factors distort the figures. Many of those who contracted Ebola sought solace not from doctors, but from faith healers, further exacerbating the situation. Even as rumours began to circulate that Ebola was spreading to cities in Liberia and Sierra Leone, officials high up in the WHO denied the danger. As late as June 2014, over six months from the start of the outbreak, they were still refusing to declare an international crisis – and then flights to west Africa were abruptly cancelled. Meanwhile, corpses were piling up in the streets of Monrovia. Monsoons made the situation completely disastrous, with heavy rains causing the hastily buried dead to float back up to the surface.
The world only woke up to the disaster when several cases were reported of sick people travelling by plane to various destinations, including the US.
In the end, international resources made a difference. But the epidemic would not be quelled completely for more than 19 hellish months after the WHO declared an international public health emergency. Ebola affected nearly 30,000 people, and cost the lives of 11,000.

This monster will be back again
Honigsbaum writes that Ebola made the world painfully aware that the appearance of new pathogens in previously remote areas posed a growing risk. Like the terrorist attacks of 11 September 2001, Ebola showed how porous the airspace makes the world and how vulnerable it is to exotic diseases, which can be anywhere within 72 hours.
But Ebola also confronted scientists with the enormous unpredictability of these types of viruses. How on Earth could “Zaire Ebola” end up all the way in Guinea, 5000km away? Fruit bats are thought to be the culprit, but that has not been confirmed.
Gorillas and chimpanzees can also carry the virus, and all these animals are hunted for food. Moreover, there are a number of different strains of the Ebola virus that we know of – some deadlier than others – that have been found in various places (including Reston, Virginia). That variety also presents researchers with a perplexing riddle. Worse yet, no one knows where the virus hides between outbreaks and what happens to it.
The Hot Zone presents the mystery in dramatic fashion. Once the immediate danger appears to have been averted, lead scientist and army veterinarian Nancy Jaax (played by Julianna Margulies) takes the stage. As the military pathos swells in the background score, she warns the world: “The Ebola virus feeds and then it retreats back into the shadows, where it learns, mutates. Believe me when I tell you, this monster will be back again and we need to be ready.”
That may sound somewhat alarmist, possibly even populist. But one line from the series finale kept echoing in my mind as I read Honigsbaum’s book with growing amazement: “You could say that Earth’s immune system has finally recognised its most destructive pathogen: humans.”
Dig deeper
 Why Covid-19 is not like the flu (and eight other key insights from experts)
The amount of information about coronavirus is overwhelming. So we organised a live chat with experts from around the world on 24 March. Here were the nine key points.
Why Covid-19 is not like the flu (and eight other key insights from experts)
The amount of information about coronavirus is overwhelming. So we organised a live chat with experts from around the world on 24 March. Here were the nine key points.