The coronavirus pandemic has changed life as we know it. There is still a lot we don’t know about the virus itself, so we organised a Q&A with renowned experts from all around the world to answer your most pressing questions.
Here are nine key insights from a wide-ranging, informative chat. You can also click on a number to jump straight to that section.
- Covid-19 is not like the flu
- You spread the Sars-CoV2 virus in two ways
- It will take two weeks for you to see symptoms (if you see any at all)
- Contact your doctor if you have symptoms and suffer from underlying health conditions
- You have the next few weeks to prevent transmission
- You should not consider masks to be your biggest priority
- By ‘flattening the curve’, you are helping your healthcare system
- We might see a second wave of cases – even in the summer
- It’s unclear how long this will last
Thank you to all the experts and members who participated, and stay safe!

Covid-19 is not like the flu
Sars-CoV2 is the name of the virus, and this causes the disease Covid-19.
This disease is not like the flu, says William Hanage, associate professor of epidemiology at Harvard’s school of public health.“Coronavirus is caused by a different virus, the properties of which we are only beginning to understand.”
So what do we know? Kate Tulenko, a US physician, points out that the virus is different from viruses causing the flu because:
- it is easier to transmit;
- there are no verified treatments yet;
- there is no vaccine yet;
- it appears to be 10 times deadlier than the flu.
Nassim Assefi, an Iranian-American internist and global health specialist based in Morocco, echoed Tulenko in pointing out “the novel coronavirus is different from the flu. It belongs to a different class of coronaviruses, of which there are around six/seven known to transmit to humans. And because it is a novel (new) virus, “there is no herd immunity to it yet”.
“Pandemics have occurred occasionally throughout history,” Ben Cowling, professor in infectious disease epidemiology, School of Public Health, the University of Hong Kong, explained to Greta, a member who wanted to know how we could stop this from happening again. “In many cases they originate from wild animals (for example Covid-19, HIV, and some influenza pandemics). In other cases, they originate from domestic animals (like swine flu). We can reduce the risk of pandemics by reducing the opportunities for transmission of infections between wild animals and humans.”
You spread the virus in two ways
Firstly, you get the Sars-CoV2 virus “from breathing in the same air that an infected person has breathed out. [This is] particularly risky if you breathe in the air that they just coughed out. If you stay 1.5 metres [4.92 feet] away from other people, you would be too far away to breathe in the contaminated air that they have breathed out, and too far away to be infected if they coughed in your direction,” explained Cowling.
The second way is “from a virus that has gotten in the environment, for example on a door handle, and you touch it and then touch your mouth or nose. That is why hand hygiene is so important.”
It will take you up to two weeks to see symptoms (if you see any at all)
“The incubation period, the time from infection to developing symptoms, is about two weeks,” explained August Lindmark, a doctor at Yale New Haven Hospital and the Yale School of Medicine in the US. “That’s the longest possible period estimated. The average incubation period that a given person experiences is 4-5 days in the studies that are currently available,” said Lindmark in a message after the chat. He added it’s important to know that you can still transmit the infection even when no symptoms are present.
What are the symptoms?
“Fever, fatigue, and cough are the most common symptoms,” Lindmark explained. “Less common symptoms include sore throat, headache, as well as gastrointestinal symptoms like diarrhoea and nausea.”

Contact your doctor if you have symptoms and suffer from underlying health conditions
The next few weeks are critical, explained William Hanage, associate professor of epidemiology at Harvard University.
“We expect a surge (in places where community transmission has taken off) that will test healthcare facilities.” If you show any of the symptoms described above, “contact your doctor for advice, and do everything you can to avoid infecting anyone else.”
As a doctor on the frontline, Lindmark agreed:
“First and foremost, contact your primary care clinician and/or local Covid-19 hotline for next steps. Your clinic may set up a telehealth visit or have special protocols for evaluating people. This is a general FAQ that we use at Yale for ‘what to dos’. Look for a similar document that applies to your community, health system, or clinic.”
You have the next few weeks to help prevent transmission
“It is correct to say that [population immunity] will help prevent transmission,” said Hanage. “For an infection like this, you would need around half of all people to be immune to start to bring it under control. The doubling time seems to be a little under a week, so cases will climb quickly without controls.”
That is why about 20% of the world’s population have been ordered to stay at home. “Measures to try and stop transmission now (social or physical distancing) are intended to reduce strain on healthcare in the future. If we can stop roughly half the transmission events, we can start to bring this under control,” said Hanage.
Cowling reminded us that the distancing measures in place “are intended to stop people becoming infected now who will be needing life saving care in about a month. If large numbers become infected, this will lead to excess mortality. It is hard, to say the least, to project beyond then. However, if we find the population level immunity has built to the point that we no longer expect outbreaks, then things can be relaxed.”
Yet even in Wuhan, where restrictions are to gradually be lifted from April 2020, “many in the city don’t think it is time to celebrate or to let their guards down just yet, in fear of a second wave,” said Yuli Yang, a journalist whose family has been on lockdown in Wuhan for the last two months. “Many people in Wuhan I spoke to say that they plan on staying indoors as much as they can and continue on the safety routines they have established under the months’ long lockdown whenever possible.”

You should not consider masks to be your biggest priority
“There may be evidence the virus is airborne for longer periods of time, that’s why many health workers are using N95 masks when caring for patients,” said Lindmark.
But, as Cowling pointed out, “we should prioritise supply for healthcare workers above the general community.” And: “I think homemade masks might be able to provide some protection against infection in the community, but it would be even better to stay at home and avoid crowded areas.”
Cristina Tardaguila, coordinator of the Coronavirus Facts Alliance, shared important World Health Organization guidance: “Essentially, only wear a mask if you are ill with Covid-19 symptoms (especially coughing) or looking after someone who may have Covid-19.”
Members Larry, Gabi and Russell worry about visits to the supermarket. Leysia Palen, an information scientist who pioneered the academic field of “disaster informatics”, shared a set of instructions for setting up a "decontamination station" at home.
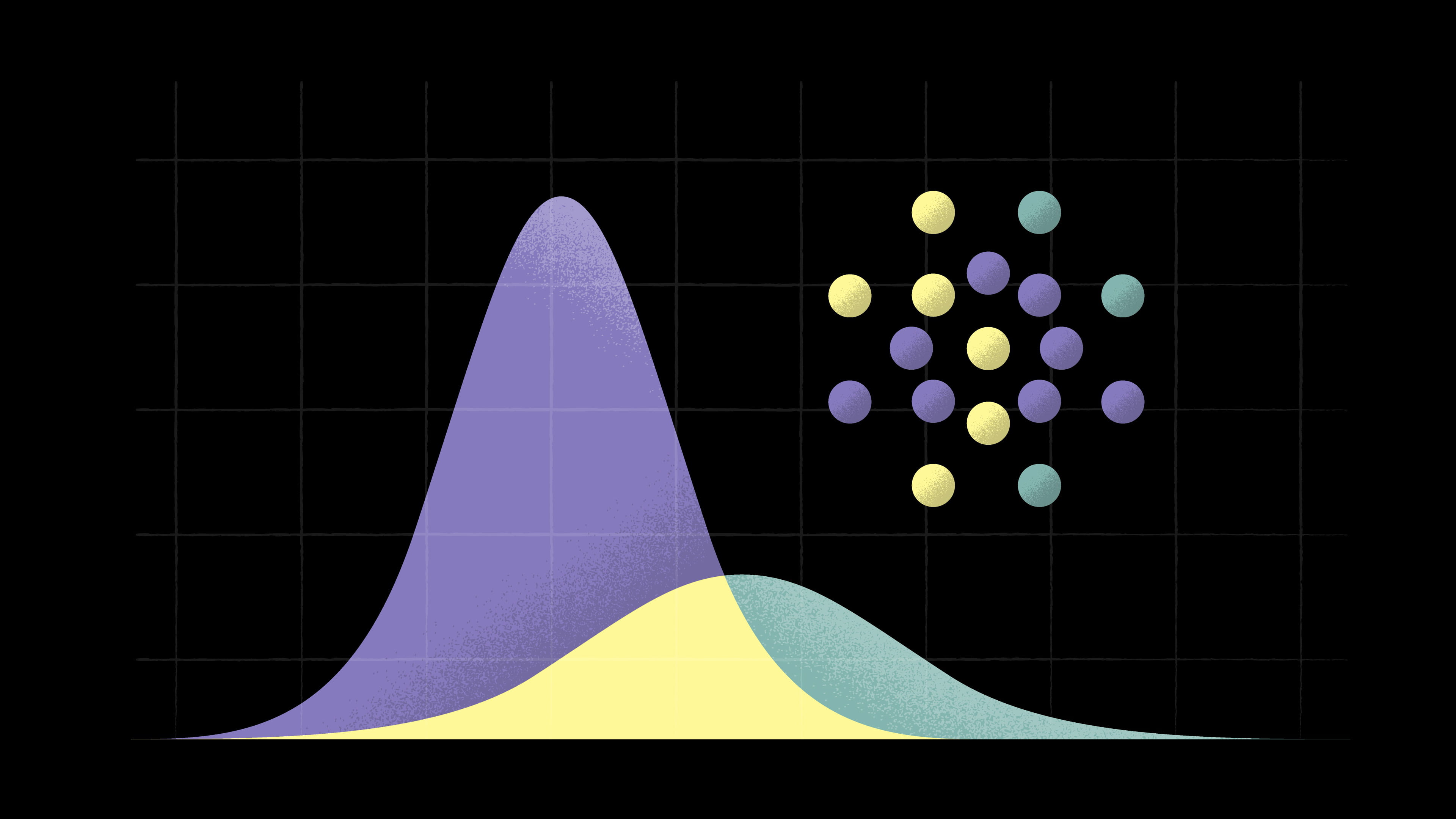
By ‘flattening the curve’, you are helping your healthcare system
At Lindmark’s hospital in Connecticut, “great care has been taken to rearrange beds, cancel elective procedures, create back-up pools of clinicians, and open space to ensure the health system’s response is as expansive and efficient as possible.”
According to Roxana Moslehi, an Iranian-American genetic epidemiologist, flattening the curve means: “Both reducing the number of cases and increasing the time in between new infections in order to allow for the healthcare system to be able to manage and treat cases effectively.”
Tulenko added that the situations in Wuhan, Milan, and Madrid showed that "many people in communities being severely ill at the same and the number of people requiring hospitalisation and ventilation will exceed the health system’s capacity. That’s why it is so important to ‘flatten the curve’ and do social distancing. That way the need for hospitalisation won’t outstrip the supply.”
Daan, a member, pointed out temporary field hospitals were already being set up in Madrid. “Ramp up testing capacity,” added Cowling. “Figure out how to use technology better to help with quarantine and social distancing.”
Kia, a member, asked if we couldn’t simply isolate those most at risk, and the rest of us go about our way. “This strategy has been considered in some countries, including the United Kingdom,” Cowling explained. “The problem is that there would still be a very large health impact. You are right that a much smaller part of the ‘young and fit’ would end up in hospital, but predictions are that this will still be a large number that will overwhelm intensive care facilities.”
We might see a second wave of cases, even in the summer
Sigrun, a member working in Burkina Faso, asked whether warmer weather made a difference to the virus surviving. Cowling responded: “We can see evidence that infections are spreading in India, Indonesia, Malaysia, and some other hot countries. Warmer weather might slow down the spread but is unlikely to prevent spread.”
Which means: summertime is not a “solution” to this pandemic.
Lindmark compared this to isolated studies which look at blood type risks. “Such data needs to be repeated, confirmed, and peer reviewed to make any substantive judgement about associated blood type risk for Sars-CoV-2. The same holds true of ambient temperature and humidity.”
Member Arya wondered if the summer months would mean that the virus will mutate.
“It is still not completely clear if or how the 1918 Spanish flu mutated between the first and second waves, and there is disagreement among experts about what exactly might have happened,” explained Cowling. “It is unlikely that Covid-19 is going to change dramatically over the next six to 12 months. There would certainly be a chance of multiple epidemic waves for locations that have relatively small first waves.”
It is not clear how long this will last
Previous pandemics and epidemics lasted for nearly two years, epidemiologist Roxana Moslehi notes.
But our experts’ estimates about the longevity of this corona pandemic varied.
“If effective treatment and vaccines become available, there is no reason we could not defeat this in closer to a year,” Moslehi said.
“I predict it’ll be a good 18 months at least,” said Nassim Assefi. “We can’t all be sheltering [at home] this whole time, but hopefully we use the time we get by staying home to make sure our health care system and its workers don’t collapse. Not to mention our economies [and our social systems].”
“I would be very surprised if [things] return to ‘normal’,” Hanage added. “You should also remember that there are a lot of things other than lockdowns that can be done. As I understand it, New Zealand has discussed four stages of increasingly impactful interventions to make it clear that some times will need more urgent action than other times.”
Dig deeper
 Deciphering the pandemic: a guide to understanding the coronavirus numbers
You’ve already read countless articles on coronavirus infection numbers. But what do those numbers really mean, and how should you read them?
Deciphering the pandemic: a guide to understanding the coronavirus numbers
You’ve already read countless articles on coronavirus infection numbers. But what do those numbers really mean, and how should you read them?