Trigger warning: this article discusses suicide and ill treatment in psychiatric care. Please do not read further if you find this topic disturbing.
Three years ago, I woke up one morning and knew that I was going to kill myself. Or, rather, I didn’t wake up since I hadn’t slept. At this point I hadn’t slept for two months, not since an adverse reaction to a new antidepressant jolted me into unending insomnia. Unable to work, I dragged myself through the days and spent my nights crying through Netflix binges. And then that morning I knew that I couldn’t live through one more single day of it.
A common refrain in campaigns to destigmatise mental illness is a reassurance that it’s okay to ask for help, but people who repeat this are often fuzzy on what exactly “help” means. In fact I had asked for help during my crisis, and was trying everything – more antidepressants, exercise, mindfulness, hot baths, good sleep hygiene, prescription sleeping pills, even journalling my way through my feelings. None of it worked. It had been a bad year up until that point, which was why I tried that fateful new antidepressant in the first place.
It felt as if that single dose of medication snapped something in my brain. Still, none of this history adequately explains why I wanted to kill myself. I felt hopeless, sure; but I’d felt hopeless before and managed to white-knuckle through it. I’d spent plenty of time during bad days, months and years thinking about death without ever giving in.
On that awful morning – the day after the summer solstice, I remember, when I’d worn a flower crown to the park and told myself I had reached a sort of cosmic turning point after which things had to get better – I just knew. Another switch had flipped in my brain.
I took a bunch of those sleeping pills that didn’t make me sleep and chased them with whiskey, wrote a note and lay down on the bed. Then, half an hour later, I knew something else: that I’d made a mistake. So I got up and took a cab to the hospital.
This is the part in the story where I want to tell you – and you want to hear – that things got better. It’s the part where there should be a nurse who was kind to me, or a doctor who tough-loved me into wanting to live.
Instead, what I experienced in the emergency room was dehumanising and traumatic. I was yelled at, accused of lying, left for hours on a bed in a public hallway. The tone adopted by most of the staff when speaking to me varied between condescension and animosity. One nurse told a doctor that I was probably a drug user because she had found a lighter when searching through my backpack. A psychiatrist kept repeating: “I don’t think you understand how serious what you’ve done is.”
The message, communicated to me by multiple staff members, said this: I wasn’t reliable when it came to telling or understanding my own experience.
It had been difficult enough to decide to come to the hospital while I was in crisis. There were moments on that day when I regretted doing so.
Inside: the terms and conditions
Maybe I’ve just been unlucky with the medical staff I encountered, but I suspect that what happened to me is much more common than most people would like to believe. It’s hard to find statistics about that specific type of experience, but we do know that coercive care is on the rise in the treatment of mental health.
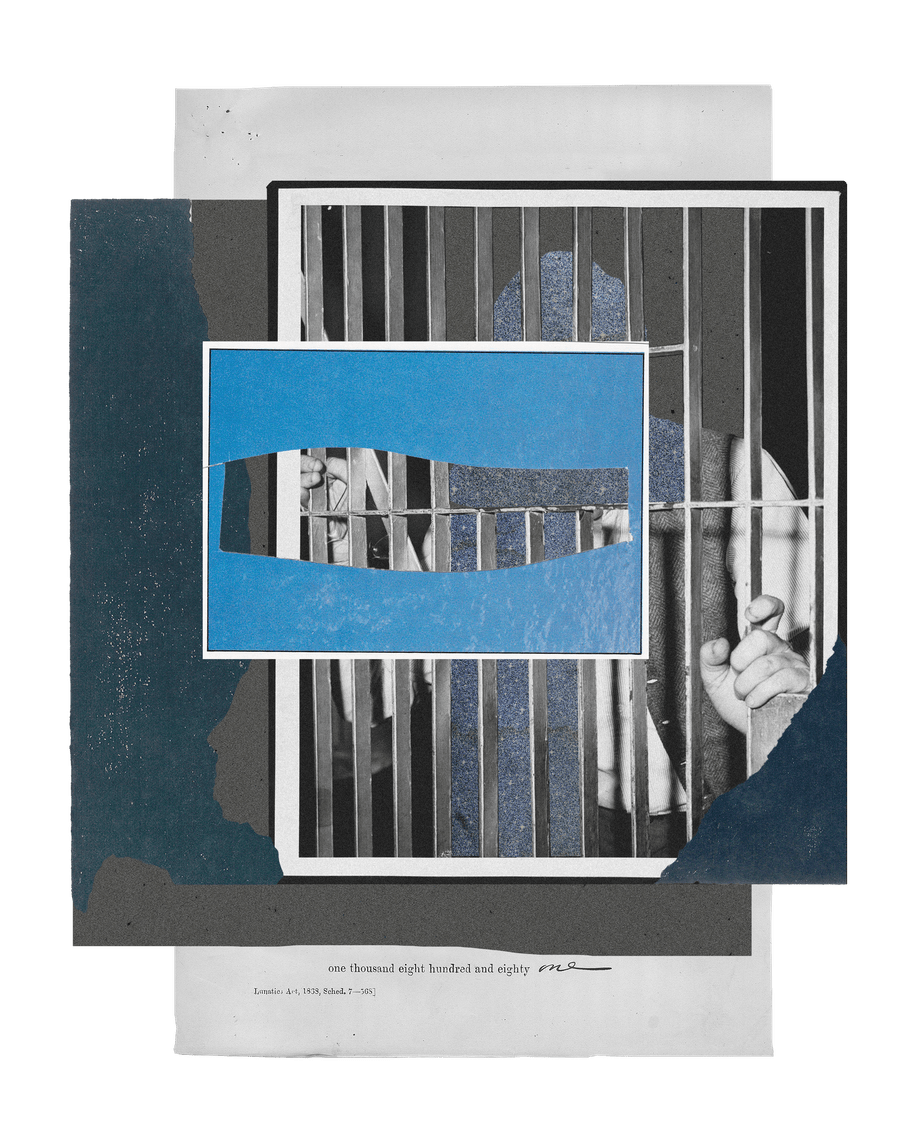
In Canada, where I live, involuntary psychiatric admissions have increased sharply in some provinces, the use of a variety of measures to hold people against their will has increased by 70-80% over the past decade. The number of certificates issued for involuntary electroconvulsive shock doubled in one province over the same period.
Involuntary admissions are also increasing in other countries, including the UK, the Netherlands, and Germany. The reported numbers likely only represent the tip of the iceberg when it comes to this issue. Journalist Anna Mehler Paperny, who assembled these Canadian statistics for an article in the Globe and Mail, points out that coercive treatment is a slippery slope: patients held involuntarily can feel pressured to agree to treatment they don’t want in the hope of clawing back some of their freedom.
A person who is too ill to recognise their illness will deny that illness. So too will someone who genuinely isn’t ill
Involuntary hospitalisation is authorised when a doctor believes that a patient cannot be safe on their own but the patient won’t agree voluntarily to be admitted to hospital. No doubt most doctors have good intentions when they choose to detain patients on a 72-hour hold, believing it’s necessary to save that person’s life. However, it’s a very paternalistic model of care that in effect compels doctors to deploy authority, to pull a power move, instead of building a rapport with their patients.
A better rapport with clinicians might help to convince a patient of the benefits of admission. Without that basis of trust, one big consequence of involuntary procedures is that the patient begins their treatment feeling unheard and disempowered. They will feel that their boundaries have been violated, as I certainly did on that day in the emergency room.
My personal experience brings into sharp relief an issue at the heart of how mentally ill patients are treated. Two concepts in mental healthcare capture this problem perfectly: the unreliable narrator and insight.
The term “unreliable narrator” was coined in 1961 by literary critic Wayne C. Booth, to describe the character who doesn’t speak or act “in accordance with the norms of the work (which is to say the implied author’s norms)”. Peter J. Rabinowitz, a professor of comparative literature, expanded this definition: “an unreliable narrator is one who tells lies, conceals information, misjudges with respect to the narrative audience – that is, one whose statements are untrue not by the standards of the real world or of the authorial audience but by the standards of his own narrative audience,” he wrote.
A fictional character might attempt, intentionally, to deceive their audience. The protagonist of Villette, by Charlotte Brontë, spends the first half of the novel obfuscating her relationship to another character, for example. Or a character’s version of reality may be inaccurate, like “Chief” Bromden in One Flew Over the Cuckoo’s Nest, a narrator whose story is filtered through his delusions and hallucinations.
A person with mental health challenges is widely believed to be someone who tells their story inaccurately. They may embellish, omit or distort. Such behaviours are sometimes written into clinical diagnoses, for example in the case of Borderline Personality Disorder for which lying and manipulation were long considered defining traits, or in disorders where people experience psychosis.
The patient can begin to question their own experience, too. In her autobiographical work Girl, Interrupted, Susanna Kaysen picks apart the events that led to her 18-month stay at a psychiatric hospital. Is what she remembers the truth, or is the version given by her doctor correct? Kaysen is able to convince herself that she doesn’t fit the trope of an unreliable narrator, by comparing notes and time stamps on various medical records. Even armed with this information, she knows that many people still won’t see her as credible.

The riddle of ‘insight’
Some part of the widespread belief that psychiatric patients can’t be trusted to tell accurate versions of their own stories has to do with the idea of “insight,” a term frequently used in psychiatry. To summarise: if a psychiatric patient knows that they’re ill, then they have insight. If a psychiatric patient denies that they’re ill (and denial can be as mild as disagreeing with a particular diagnosis), then they lack insight. A patient with insight is considered to be significantly healthier than someone who lacks it.
The problem here is not that a person who is too ill to recognise their illness will, of course, deny that illness. The problem is that so too will someone who genuinely isn’t ill. The question is set up, or framed, in such a way that the only permitted answer is: “I’m sick.”
Consequently, a patient who rejects a diagnosis is often seen as validating that diagnosis, especially if they’re already considered – labelled – a difficult patient.
If the skills to non-violently de-escalate a difficult situation with a mentally ill person can be found anywhere, surely they would be found in the staff on a psychiatric ward
During my first hospitalisation when I was 20, I was upset by a psychiatrist who interviewed me for just 10 minutes before deciding I had a personality disorder. Her belief hinged on the fact of my reluctance to tell my mother that I was in a psychiatric ward. I knew my reasons for this: my mother was several provinces away, I didn’t want to worry her, and I felt ashamed. To this psychiatrist, however, my being upset was further proof of a personality disorder. When, eventually, I offered to call my mother in front of her, she told me it was too late and that she had made up her mind. (I’ve often wondered what the right reaction on my part might have been, and I still don’t know). Once the psychiatrist had made her decision, the only way forward for me was to accept it.
My experience is that many mental healthcare practitioners turn punitive, coercive and carceral with patients who are not compliant. They can bully, threaten and sometimes forcibly confine the ones who don’t do what they want.
When I was in the psychiatric ward a few years ago, another patient became upset about missing a once-in-a-lifetime event due to her involuntary hospitalisation. Instead of working through these feelings, the staff tried to coerce her into taking medication with which she felt uncomfortable. In a burst of anger at their refusal to listen to her, she threw a tray and tried to barricade herself in her room. The episode ended with her heavily sedated and in restraints; I could hear her sobbing and moaning all evening, even from several rooms away. This episode was deeply troubling, not least because I’d believed that if the skills to non-violently de-escalate a difficult situation with a mentally ill person can be found anywhere, they would be found in the staff on a psychiatric ward. Instead, I saw serial escalation: more threats, snide comments, arbitrary revoking of privileges.
Patients who are hospitalised involuntarily have little recourse outside the system if they want to lodge a complaint. Where I live, the only authority higher than the doctor to whom patients can appeal regarding involuntary hospitalisation, is the Consent and Capacity Board. Guidance from our provincial Psychiatric Patient Advocacy Office is to apply for a hearing only as a last option. Its first advice to patients who object to being hospitalised involuntarily is “do nothing at all and allow the form to expire”.
The practical consequence is that patients seeking to speak out against the psychiatric care system are doubly silenced: first, because they are perceived as unreliable narrators; and second, because clinicians believe that prescriptive and patronising forms of care are for the patients’ own good. Both assumptions reflect how this branch of healthcare is designed: they are not flaws in an otherwise workable system.
A hierarchy of coercion
Psychiatric hospital care operates on foundational hierarchies of power. It places people who are predominantly white and male at the top, and applies clinical procedures which make it impossible to challenge their authority. Mentally ill people find themselves in a situation where questioning the way this system works is routinely interpreted by professionals as yet another symptom of the patients’ dysfunction. This hierarchy subordinates the needs of patients to the autonomy, authority – and consequently, the comfort zone – reserved for caregivers.
People want to believe that healthcare is altruistic: they need crazy people to be crazy, because this allows them to stand on the sane side of the line
Of course, there is evidence to explain all these arrangements. There are always going to be patients who can’t or won’t acknowledge that they’re ill. This is true not just in psychiatry, but across all fields of medicine. It can be heartbreaking for friends and family to watch someone deteriorate while simultaneously refusing treatment. But this fact is not adequate justification for the current system.
I believe that coercive care should be a doctor’s absolute last resort. Until that point, clinicians should focus on building a strong rapport with patients. Their trust in doctors to act with patients’ best interests in mind needs to be earned. Any care relationship that begins as, or becomes adversarial, will certainly harm the patient most.
I believe that doctors, generally, must improve their skills in listening to patients – and their capacity for believing what patients say. We almost always speak our own truth, even if that truth may not, on its surface, seem always to align with reality.
When I tell people how I’ve been treated in the mental health system, I’m often met with doubt. People have reacted with comments such as: “Maybe they were doing it for your own good”, “Maybe they just seemed angry because you were so upset” and “Maybe you’re just remembering it wrong”. It’s not just that most people tend to assume that those with mental illnesses can’t accurately report things – although, to be clear, they do certainly think that. It’s also because for many people it just feels too uncomfortable to accept that these brutal encounters occur regularly in mental health care.
As a society, we need the system to be functional for a number of reasons. Not least, I’ve noticed, is that people want to feel good about themselves for all the times they’ve told someone to get help, or referred them directly or indirectly into the system. They want to believe that healthcare is altruistic and exists for the greater good. So they need crazy people to be crazy: this allows them to draw a line, knowing that they’re on the sane side.
A clear distinction – the barrier that people imagine exists – between mental health and mental illness just isn’t real.
By the age of 40, half of all Canadians will have experienced some kind of mental illness. This is, in fact, the leading cause of disability in my home country. And if you are or end up being one of those people, I guarantee that you will want healthcare providers to take you seriously. At the very least, you’ll want them to listen.
Of course, that’s not the only reason to be concerned: you shouldn’t care about injustice only because it might happen to you. But I make this point because I find that often I don’t know how else to drive the point home. We live in a world that seems to believe that I, and others who have experienced mental illness, don’t deserve the same rights as other people.
I don’t regret going to hospital after my suicide attempt. But I can’t escape the feeling that one of the driving forces behind my commitment to staying as mentally healthy as possible is the fear of going back. I would do almost anything to avoid ending up there again. Surely the healthcare system can offer more and better motivation than fear.
If any of the issues raised in this piece resonates with you or someone you know, please know you don’t have to suffer in silence. Seek help.
Dig deeper
 Knowing our ‘mad’ ancestors: why it’s time to look again at mental illness in history
It’s important to know the stories of people who have suffered mental illness but historical representation can be tricky. We should look to the stories not to find the ways they were exceptional, but the ways in which they were mundane.
Knowing our ‘mad’ ancestors: why it’s time to look again at mental illness in history
It’s important to know the stories of people who have suffered mental illness but historical representation can be tricky. We should look to the stories not to find the ways they were exceptional, but the ways in which they were mundane.
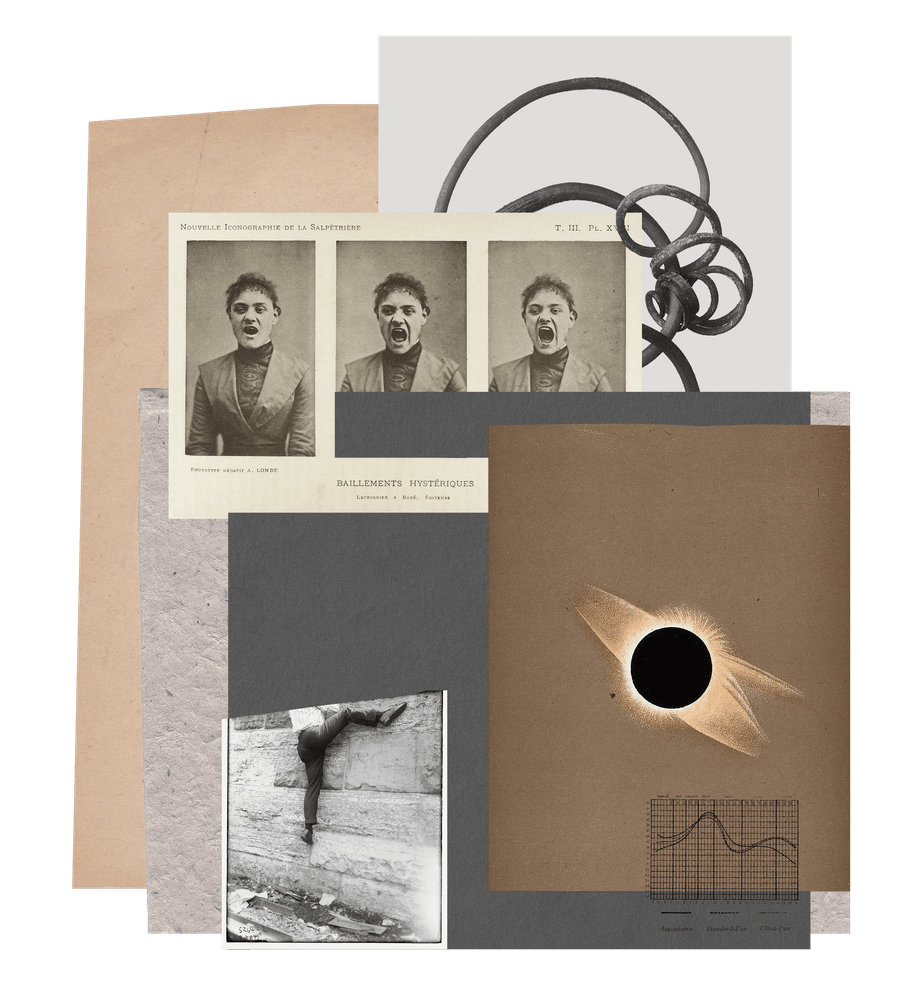
 Better than bloodletting? Despite centuries of change, the treatment of mental illness remains largely the same
Bloodletting, purging, and cold baths may no longer be common practices in psychiatric care, but the most important evolution – towards patient-centred treatment – has yet to happen.
Better than bloodletting? Despite centuries of change, the treatment of mental illness remains largely the same
Bloodletting, purging, and cold baths may no longer be common practices in psychiatric care, but the most important evolution – towards patient-centred treatment – has yet to happen.